Advancing Maternal and Infant Health Research Through Data Interoperability
Posted in Blog What's New
May 2025
By Aditi Bhardwaj, MS
Introduction
In an increasingly data-driven healthcare environment, the seamless exchange of patient information—known as data interoperability—has become essential for improving care coordination, efficiency, and outcomes. Interoperability ensures that data is consistently structured and understood across systems, enabling providers to deliver more informed and timely care decisions (Office of the National Coordinator for Health Information Technology, n.d.).
This need is especially critical in perinatal health, where the care journey often spans multiple providers, specialties, and systems. Through our work on the Safe Babies Safe Moms (SBSM) initiative in Washington, DC, a value-based care program focused on improving maternal and neonatal outcomes, we encountered firsthand the barriers and opportunities surrounding interoperability. As part of the Health Care Financing Initiative (HCFI), our team explored data challenges that affect the financial sustainability of such programs—including the need for better patient risk stratification, gaps in billing data, and the difficulty of integrating disparate data sources.
The broader literature underscores these experiences: studies consistently link interoperability with improved participation in alternative payment models (APMs) and stronger care coordination (Holmgren et al., 2022; Drozdowicz, 2023). Yet, persistent obstacles—such as data silos, incompatible systems, and privacy concerns—continue to hinder meaningful progress (Blavin et al., 2015). Overcoming these hurdles requires coordinated effort among policymakers, providers, vendors, and standards organizations.
Building a Holistic Perinatal Dataset
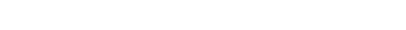
A core objective of SBSM was to construct a comprehensive, longitudinal dataset capturing the full perinatal experience. Our vision included data on health history, utilization patterns, cost of care, and outcomes for both mother and baby, creating a detailed picture of each pregnancy episode. Importantly, this dataset went beyond the maternity department to include information from across MedStar Health, unified under the mother-baby dyad as the analytical unit.
While true cross-provider interoperability remains the ideal, we focused on integration within a single health system to respect HIPAA and privacy regulations. This still presented significant challenges—linking billing, clinical, and appointment data across departments—but ultimately enabled a unified, system-wide view of perinatal care.
Figure 1. Integrating Diverse Data Sources to Build the Mom-Baby Dyad Dataset
Bridging Data Gaps: A System-Wide Approach
The SBSM initiative relied on combining data from several key sources within MedStar Health:
- Billing Systems, which provided detailed cost information for maternal and neonatal services. This data had to be standardized and mapped for accurate cost analysis.
- Clinical Data Systems, which housed diagnosis and treatment records for both mothers and babies across the care continuum.
- Appointment Systems, which tracked encounters before, during, and after pregnancy, offering context for both preventive and follow-up care.
By bridging these internal silos, we created an integrated view of the perinatal journey. While this only reflects data from within one health system, it demonstrates what’s possible when internal interoperability is prioritized.
Looking Forward: Laying the Foundation for Next-Generation Perinatal Analytics
Our work integrating maternal and neonatal data was not just about technical consolidation—it was about unlocking new insights to guide care innovation. The resulting dataset positions us to explore trends across the full perinatal episode and assess the effectiveness of interventions in ways that weren’t previously possible.
Looking ahead, this foundation will support more robust evaluation of care models and drive quality improvement in maternal and infant health. More importantly, it offers a model for how value-based programs can use data integration to improve outcomes and inform health policy.
Achieving broader interoperability across health systems remains a challenge, but initiatives like SBSM show how progress can be made—even within complex data environments—by focusing on internal integration and building toward scalable solutions (Joynt & Jha, 2014; Centers for Medicare & Medicaid Services, n.d.).
References
- Blavin, F., et al. (2015). Overcoming barriers to health data interoperability. Health Affairs, 34(9), 1560–1567.
- Centers for Medicare & Medicaid Services. (n.d.). Value-based programs. https://www.cms.gov/medicare/quality/value-based-programs
- Drozdowicz, L. (2023). Interoperability and participation in alternative payment models. Healthcare Policy Review, 17(2), 54–72.
- Holmgren, A. J., et al. (2022). The role of interoperability in value-based care. Journal of Health IT, 45(3), 112–128.
- Joynt, K. E., & Jha, A. K. (2014). The financial effect of value-based purchasing and the hospital readmissions reduction program on hospitals in the United States. Annals of Internal Medicine, 161(12), 760–762. https://doi.org/10.7326/M14-2813
- Office of the National Coordinator for Health Information Technology. (n.d.). United States Core Data for Interoperability (USCDI). https://www.healthit.gov/isp/united-states-core-data-interoperability-uscdi