Stewardship & Sustainability: An Economic Evaluation Plan for Pediatric Food Security and Financial Health Interventions

Posted in SDOH What's New
May 2025
Authors: Carol B. Davis, PhD, MBA – Assistant Research Professor & Associate Director
Emmanuel Carrasco Hernandez, MPP – Research Assistant
Emmanuella Sobo, MPH – Research Program Manager
All authors are affiliated with the Health Care Financing Initiative Research Center at the McCourt School of Public Policy at Georgetown University.
Introduction
The Department of Community Pediatrics (DCP) at MedStar Health provides pediatric primary care through the Kids Mobile Medical Clinic in Washington, DC. Routine social determinants of health (SDOH) screening in 2022 showed that 32% of DCP patients experience food insecurity, highlighting both the urgency of intervention and opportunity for innovation.
Building on successful pilot programs focused on addressing food insecurity and an established medical-legal partnership clinic, DCP aims to expand its role as a hub for pediatric health and related needs. These early efforts lay a strong foundation for integrating social care into medical practice and offer a real-world setting for broader, multidisciplinary evaluation.1
Our health economics team was invited to lead the healthcare finance research effort. We will conduct a focused evaluation of the program’s financial feasibility, cost-effectiveness, and return on investment (ROI). This work is part of a larger collaboration to assess the long-term viability of the health-related social needs (HRSN) interventions integrated in pediatric primary care at MedStar and explore its potential as a model for scaling and sustaining similar programs elsewhere.
📄 Download the full handout (PDF)
Click here to access it. Includes the full evaluation framework, references, and institutional acknowledgments.
Background
Anecdotal evidence and a growing body of studies are generating increased interest in integrating SDOH and HRSNs into pediatric healthcare settings. Research suggests that interventions targeting food security and financial health can reduce food insecurity by 14–25% and increase adherence to well-child visits by 35–60%.2 Cost-benefit projections estimate that every $1 invested in such interventions could yield up to $0.85 in savings over five years,2 through reduced healthcare costs, improved preventive care, and more efficient use of social services.2
Despite this promise and the growing enthusiasm for testing and studying SDOH/HRSN integration in clinical settings,3-5 there is still no clear mandate to make these interventions a permanent part of healthcare delivery or insurance budgets. Published reviews reveal a need for more evidence, stronger research designs, and clear policy or business frameworks that attribute the impact of interventions on health or health-related outcomes. This will strengthen the case for scaling and financially sustaining such programs in healthcare.2-3, 6-7
Additionally, there is limited guidance on how to structure or scope the role that providers or payers should play in addressing patients’ HRSNs. There is also little direction on how providers, partners, and other sectors should share responsibility. This gap is particularly evident when seeking evidence to build a rationale to allocate resources across traditional siloes of financial responsibility.
…to assign economic value to program outcomes within a policy-relevant time horizon and demonstrate that the value could be repeated, scaled, and adapted in other settings.
Methods
Our evaluation approach began with traditional economic measures—program cost and cost-effectiveness—but was expanded to address broader goals and the overlapping expectations of multiple stakeholders. Our mandate required more—this plan needed to assign economic value to program outcomes within a policy-relevant time horizon and demonstrate that the value could be repeated, scaled, and adapted in other settings.
We conducted an interdisciplinary review of scholarship spanning health services research, global development economics, public choice economics, public health, and business performance management. This foundation helped us develop an evaluation approach attuned to both fiscal outcomes and the organizational capabilities that underpin sustainable performance.
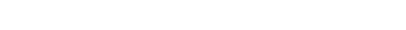
We adopted the Balanced Scorecard framework to link financial, operational, and implementation goals. This framework also supported integration with the clinical implementation and community-based participatory research strategy of our broader project team. These elements are being operationalized in a conceptual model and analytical toolkit to estimate the performance and potential of implementing the intervention at MedStar DCP over a five-year period—grounded in practical insights and critical analysis.
STEWARDSHIP & SUSTAINABILITY FRAMEWORK
Economic Evaluation of Food and Financial Health Interventions in Dept. of Community Pediatrics
The Food as Medicine (FAM) program aims to increase access to healthy food and reduce food insecurity, thereby improving participants’ nutrition and health outcomes. The Medical Financial Partnership (MFP) program focuses on reducing financial stress, improving financial well-being, and addressing unmet social needs through financial health screenings and support services for lowincome families. Together, these programs enhance the capacity of DCP as a hub and anchor for the families and children they serve and advance the development of sustainable models for replication and scalability in other local communities. The Stewardship and Sustainability Evaluation is to plan to demonstrate the value and financial viability of the FAM and MFP programs, in alignment with the concerns of patients, providers, and funders.
The Stewardship & Sustainability plan addresses several imperatives:
1. Refine the conceptual pathway connecting health, health-related needs, social intervention, financial and social value to specific customers to deepen understanding of how and to whom healthcare and SDOH integration generates measurable outcomes.
2. Address persistent gaps in the healthcare/HRSN integration literature, particularly concerning the robustness of evidence and inclusion of data regarding economic cost, program impact, attribution, and generalizability.
3. Evaluate implementation outcomes alongside the organizational capabilities that enable repeatability, scalability, and transferability.
4. Account for multiple perspectives—patients, providers, funders—when reporting the economic case for incorporating HRSNs, specifically food security and financial health into pediatric primary care.
5. Establish benchmarks and targets using external and internal comparisons.
This economic evaluation is embedded within a broader SDOH design and research effort led by MedStar Health Research Institute and MedStar Department of Community Pediatrics. The team’s commitment to collaborative practice and participatory research has shaped every stage of this work.
Implications for Policy & Practice
The Stewardship and Sustainability banner reminds us that the economic evaluation must reflect the effectiveness of delivery models designed to scale, adapt, and serve the interests of patients, providers, and sponsors—while also identifying spillover benefits that may attract future partners. It is equally important to define the role of healthcare providers—as anchors, actors, and advocates—so their contributions complement public and community resources while remaining aligned with their core responsibility: maximizing the impact of limited resources for promoting health.
Over the next 3–4 years, our empirical research will strengthen the evaluation framework and generate evidence on the potential of the DCP/SDOH model to support integration of upstream interventions into pediatric primary care. DCP is well-positioned to lead the next generation of pediatric SDOH innovation and evaluation. This stewardship model contributes a balanced economic evaluation alongside a community-based participatory research (CBPR) approach, ensuring responsiveness to both health system priorities and community needs.
…health care providers…complement community resources…aligned with core responsibility to maximize impact of resources for promoting health
Acknowledgments
Our work is part of the Social Determinants of Health Innovation and Resilience Research Project. Dr. Janine Rethy, MD, MPH, and Joanne Odom, LICSW lead an interdisciplinary team from MedStar Dept. of Community Pediatrics, MedStar Center for Health Equity Research, Health Justice Alliance (GU Law) and our Health Care Financing Initiative (GU-McCourt). Financial support is provided by the J. Willard and Alice S. Marriott Foundation.

Suggested Citation
Davis CB, Carrasco Hernandez E, Sobo, E. Stewardship & Sustainability: An Economic Evaluation Plan for Pediatric Food Security & Financial Health Interventions. Poster presented at MedStar Health – Georgetown University Research Symposium, May 2025, Bethesda, MD
References
1. Johnson, Nichelle, Odom, Joanne, and Rethy, Janine A. Healthy Children and Families: Understanding and addressing the complex interplay of food insecurity and child health. Food as Medicine Program. Internal Presentation. February 2024
2. Nikpay, Sayeh, et al. Return on Investments in Social Determinants of Health Interventions: What Is the Evidence? Health Affairs Scholar, August 2024
3. Stahacz, Charlotte, et al. The Impact of Food Aid Interventions on Food Insecurity, Diet Quality and Mental Health in Households with Children in High-Income Countries: A Systematic Review. Public Health Nutrition, June 2024
4. Schickedanz, Adam, et al. Clinic-Based Financial Coaching and Missed Pediatric Preventive Care: A Randomized Trial. Pediatrics, March 2023
5. Hinton, Elizabeth, and Amaya Diana. Section 1115 Medicaid Waiver Watch: A Closer Look at Recent Approvals to Address Health-Related Social Needs (HRSN). KFF (blog), March 2024
6. Fichtenberg, Caroline M., et al. Improving Social Needs Intervention Research: Key Questions for Advancing the Field. American Journal of Preventive Medicine, December 2019
7. Birkenmaier, Julie, et al. Medical-Financial Partnerships for Improving Financial and Medical Outcomes for Lower-Income Americans: A Systematic Review. Campbell Systematic Reviews, September 2024
8. Kaplan, Robert S., and David P. Norton. The Balanced Scorecard—Measures That Drive Performance. Harvard Business Review, February 1992