Data Signals for Economic Analysis of Maternal Mental Health
Posted in Uncategorized
As part of our ongoing work on maternal mental health within the Safe Babies Safe Moms (SBSM) initiative, we identified a pattern in the data that prompted an important methodological question — not a conclusion, but a pause.
Across our sample (N = 3,144), approximately 22% of birthing persons screened positive on the EPDS, while about 18% had a documented maternal mental health condition (MMHC) identified through ICD-10 diagnosis codes. While these figures are directionally similar, a closer look shows that they do not represent the same individuals.
A Closer Look: Screening (EPDS) vs. Diagnosis (ICD-10 codes)
To better understand this disconnect, we examined the relationship using a simple 2×2 matrix based on percentages rather than raw counts (Figure 1).
(
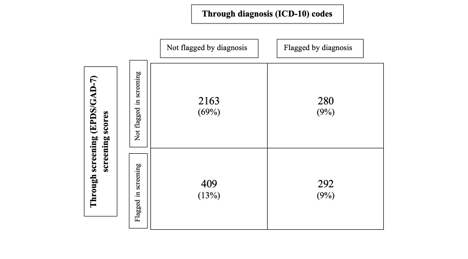
- ~13% screened positive on EPDS but had no MMHC diagnosis
- ~9% had an MMHC diagnosis but did not screen positive on EPDS
- ~9% were identified by both screening and diagnosis
- ~73% were identified by neither pathway
The overlap exists, but it is far from complete. A meaningful share of individuals appear in only one system, highlighting that screening-based and diagnosis-based identification capture overlapping but distinct populations.
Why This Matters
Screening, diagnosis, and treatment are often treated as interchangeable signals in research, yet they represent distinct steps along a care pathway. Depending on which signal is used, estimates of prevalence, service use, outcomes, and costs may differ — potentially obscuring unmet need or mischaracterizing impact.
This distinction is particularly important considering our prior literature review, Maternal Mental Health as a Contributor to Adverse Perinatal Outcomes: Observations from Prior Literature (see here), which highlights how maternal mental health conditions are associated with substantial long-term non-medical costs, including effects on employment, caregiving capacity, and family well-being. The misalignment observed here underscores why careful measurement matters: understanding who is identified — and how — directly shapes how these downstream impacts are quantified and interpreted.
Why This Is Worth Further Study
At this stage, we cannot determine whether this misalignment reflects differences in timing, workflow, documentation, or care pathways — nor do we attribute it to any single data or system issue. What we can say is that the divergence is consistent, visible in the data, and large enough to matter.
More broadly, this finding raises questions for the literature, where studies often rely on a single indicator without distinguishing between screening, diagnosis, and treatment. Understanding how individuals move across these pathways is essential for accurate measurement and meaningful policy insight.
Ultimately, this finding underscores a core challenge in health services research: before asking what outcomes cost, we must be confident we understand who is included in the data — and who is not. Our next steps will focus on disentangling these pathways, with the goal of better aligning screening, treatment, and measurement to support more accurate evaluation and policy-relevant insight. This is not a conclusion about failure or effectiveness, but a data signal — one that suggests the need for more nuanced measurement of maternal mental health pathways.