August 6
Posted in Blog
Small-Area Geographic Variation in Long-Term Acute Care Hospital Capacity: Differences Merit a Closer Look for Implications for Access, Choice and Quality of Post-Acute Experience
by Carol B. Davis, PhD, MBA
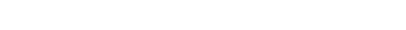
At HCFI, our team has been collecting perspectives and insights on post-acute care, in light of the public health emergency. In that vein, an article in Health Affairs inspired us to consider the topic of geographic variation in Medicare spending as potential evidence of variation in access to specialized care settings. Researchers in that Health Affairs study observed a narrowing of small-area Medicare spending growth between 2007 and 2017, and they found an inverse relationship between small-area Medicare spending growth, and the availability of certain post-acute providers. The findings contribute to the growing body of literature concluding that the supply, geographic distribution, as well as patient transfer patterns from acute to post-acute care settings are important drivers of Medicare spending growth. Narrowing the variation in spending, they reiterate, remains a necessary goal of Medicare payment reforms.
The ongoing COVID-19 pandemic offers an important context within which to interpret that reminder. During times of peak demand, limited availability of vital specialized personnel, facilities, and equipment can be strategic community health assets. The array of PAC providers in the region could certainly affect practical access to the care setting most suited to treatment goals for each patient.
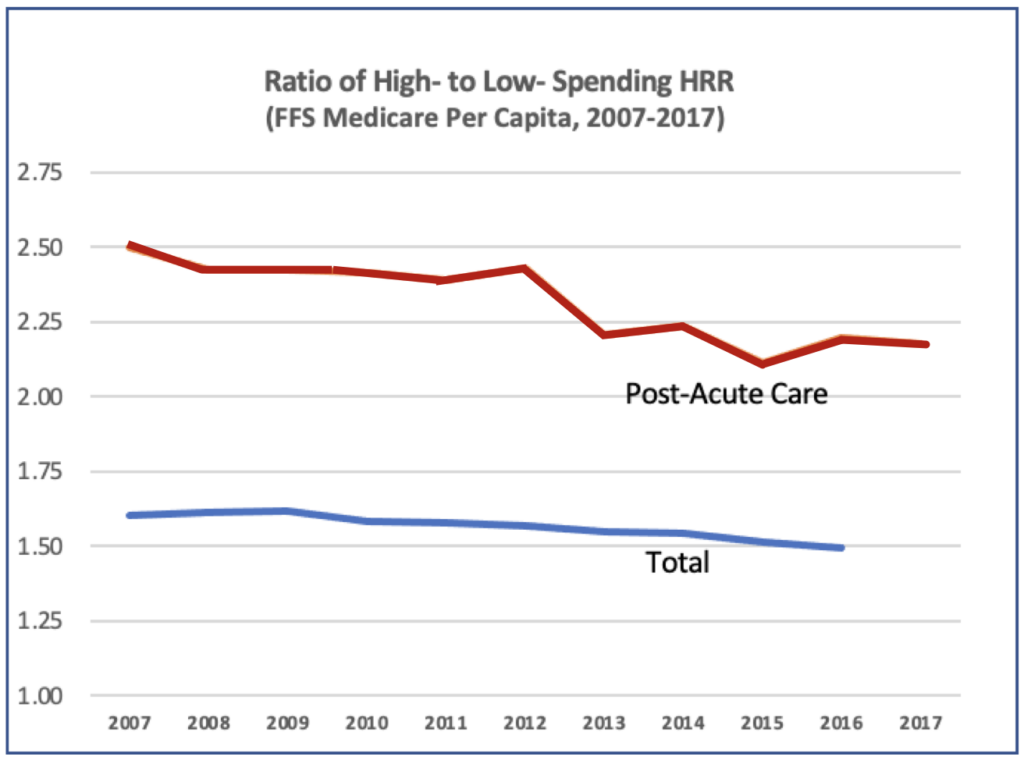
Using the Mid-and South-Atlantic states as a case study, our HCFI team took a closer look at the availability of long-term acute care hospitals, comparing the capacity to expected demand, to investigate whether the differences across referral regions is substantial enough to influence discharge transfer decisions, outcomes cost. To that end, the subject of long-term acute care hospitals is an interesting starting point for a current assessment of geographic coverage and access to specialized care.
Long-term acute care hospitals are intended for a very specific purpose—to care for medically-complex patients, who require an extended period of acute hospitalization, and often with respiratory system failure, sepsis, or other organ failure. LTCH patients are not yet in the recuperation phase of their illness when they leave general hospitals. LTCH staff and facilities are skilled and equipped to provide critical care, for patients who were required respiratory support and/or spent days in the intensive care unit. We wondered about the landscape of these specialized facilities, whose clinical capabilities, personnel, and experience must be of great relevance during a global pandemic of an evolving respiratory virus like COVID-19.
Our HCFI team conducted an analysis of LTCH availability in the Mid-and South-Atlantic to explore this topic. “While overall capacity appears more than adequate to serve the expected demand for LTCH admissions in normal times, the small-area capacity relative to local demand exhibits a great disparity. Four of fifty-six hospital referral regions (HRR) had LTCH capacity 10 times expected Medicare FFS demand. At the same time, nearly one-third of the referral regions had no LTCH beds at all”.
Mid-and South-Atlantic Hospital Referral Region, 2018
The pandemic provided stark evidence of the limits to substitution across the levels of post-acute providers, and a reminder that ongoing policy reforms must balance cost-saving goals with policies that help identify and remedy undersupply of resources where deficits exist.
Many anticipate that issues of unequal access and unequal outcomes will remain in the fore of policymaking even after the pandemic subsides. If that is the case, the geographic availability of highly-specialized services, such as post-acute hospitals, and the need for policy to remove barriers to care regardless of insurance or geography, may well come into the spotlight.
Read our full report .
#PostAcuteCare # GeographicVariation # Medicare #HealthcareDelivery #Access